Summary
Sleep deprivation is one of the most underrated causes of skin inflammation. When you don’t sleep deeply—or your sleep is fragmented by light, stress, temperature, or poor sleep habits—the body increases inflammatory signaling pathways, elevates cortisol, weakens the skin barrier, slows healing, and disrupts microbiome balance. Dermatologists now recognize chronic sleep loss as a major driver of acne flares, redness, eczema irritation, rosacea sensitivity, puffiness, and premature aging. The strongest way to reduce sleep-driven inflammation is to improve sleep quality, not just sleep duration. This means blocking nighttime light, stabilizing circadian rhythms, supporting melatonin, and protecting deep sleep. A total blackout mask—especially a 3D contoured blackout mask like the Nidra Total Blackout Mask—is one of the most effective tools because it ensures true darkness, reduces nocturnal micro-arousals, and protects the hormonal repair window required for inflammation control.
Introduction
Inflammation is at the root of almost every visible skin problem: breakouts, puffiness, redness, dullness, flaking, eczema irritation, sensitivity, and signs of premature aging. But the conversation about inflammation typically focuses on UV exposure, diet, skincare products, stress, and environmental pollutants. One of the most powerful inflammatory triggers, however, is rarely discussed: sleep deprivation.
Dermatologists worldwide now emphasize that poor sleep is an independent risk factor for chronic inflammation—not just in the body, but specifically in the skin. When sleep is disrupted, slow-wave (deep) sleep shortens. When deep sleep shortens, inflammatory cytokines rise, cortisol becomes dysregulated, and the skin barrier weakens. This cascade makes the skin more reactive to irritants, more prone to redness, more inflamed, and slower to heal.
This article explains the biological relationship between sleep and skin inflammation, what dermatologists want consumers to understand, and the evidence-backed strategies that reduce inflammation overnight—starting with total darkness and circadian alignment.
Why Sleep Deprivation Triggers Skin Inflammation: The Biological Breakdown
-
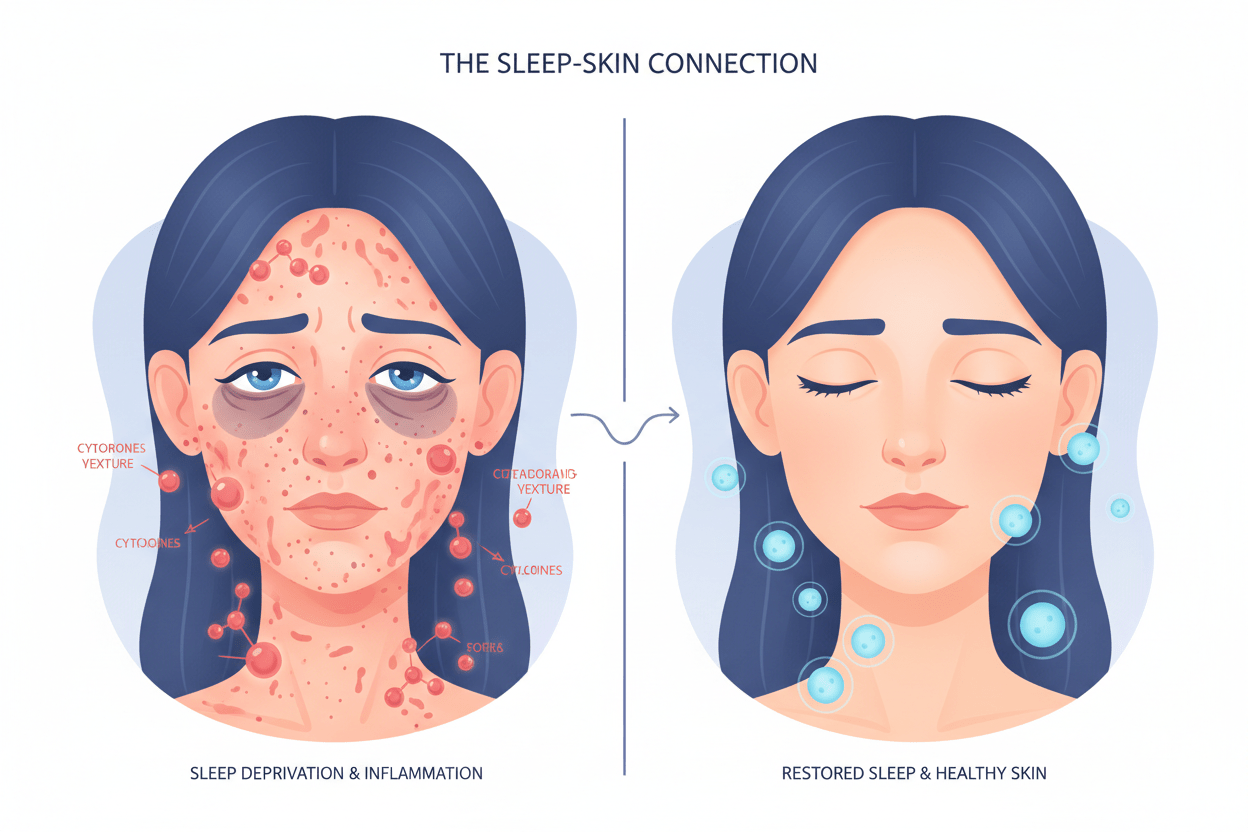
Sleep Loss Increases Systemic Inflammatory Cytokines
When sleep is restricted—even for one or two nights—the body increases the production of inflammatory cytokines such as IL-6, CRP, and TNF-α. These are the same biochemical markers that flare eczema, worsen acne, and increase facial redness and swelling.
Key impacts on skin:- More inflammatory breakouts
- Exacerbated eczema or dermatitis
- Higher baseline redness
- Increased swelling and puffiness
- Slower healing
- Sleep loss elevates inflammatory markers IL-6 and CRP [Irwin 2015].
- Chronic sleep restriction increases systemic inflammation linked to dermatologic conditions [Irwin 2010].
-
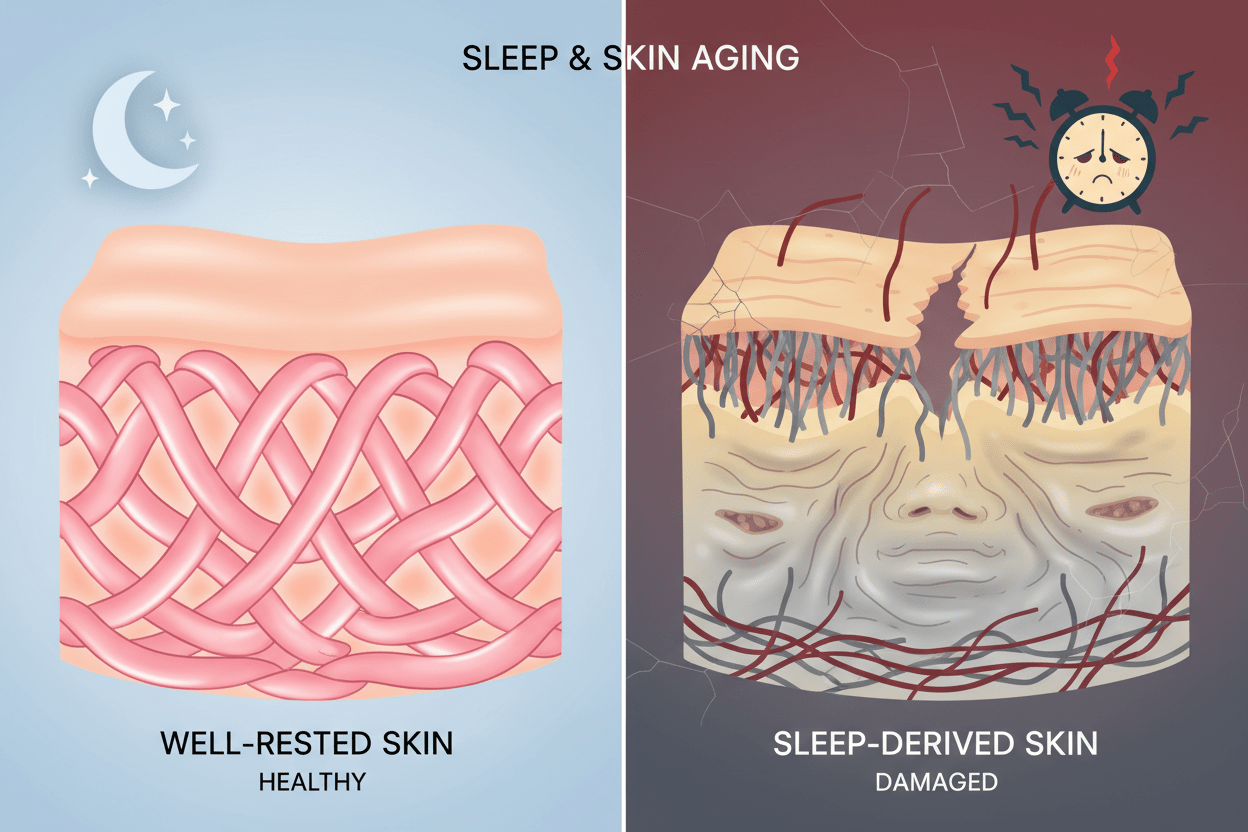
Sleep Deprivation Weakens the Skin Barrier
The skin barrier protects against irritants, allergens, pollutants, and moisture loss. When the barrier is compromised, inflammation rises sharply. Research shows that sleep deprivation increases transepidermal water loss (TEWL), indicating a weaker barrier.
Consequences:- Increased sensitivity
- Dryness and flaking
- Heightened reactivity to products
- Prolonged irritation
- Impaired wound healing
- Sleep deprivation impairs barrier function and elevates TEWL [Kim 2020].
- Poor sleep correlates with barrier dysfunction in inflammatory skin conditions [Oyetakin-White 2015].
-
Elevated Cortisol from Sleep Loss Exacerbates Inflammatory Responses
Sleep deprivation causes nighttime cortisol spikes, which suppress anti-inflammatory pathways and promote pro-inflammatory ones. Cortisol dysregulation directly contributes to acne, rosacea flares, and chronic redness.
Impacts:- Oil overproduction leading to breakouts
- Vascular dilation causing flushing
- Delayed resolution of inflammation
- Increased sebum oxidation
- Sleep loss disrupts cortisol rhythms, amplifying skin inflammation [Van Cauter 2000].
- High cortisol correlates with inflammatory dermatoses [Fisher 2002].
-
Disrupted Microbiome Balance Due to Poor Sleep
Sleep influences the skin microbiome, which regulates immune responses. Fragmented sleep alters microbial diversity, favoring pro-inflammatory bacteria and weakening protective ones.
Consequences:- Acne and folliculitis flares
- Eczema exacerbations
- Increased susceptibility to infections
- Barrier dysbiosis
- Sleep deprivation shifts skin microbiome toward inflammation [Zhang 2017].
-
Reduced Melatonin Suppresses Anti-Inflammatory Effects
Melatonin has potent anti-inflammatory properties in the skin, neutralizing free radicals and downregulating cytokines. Nighttime light exposure suppresses melatonin, removing this protection.
Impacts:- Higher oxidative stress
- Persistent redness
- Slower recovery from irritants
- Amplified UV-induced inflammation
- Melatonin reduces skin inflammation via antioxidant pathways [Hardeland 2009].
- Light at night suppresses melatonin, increasing inflammatory markers [Gooley 2011].
What Dermatologists Say About Sleep and Skin Inflammation
Dermatologists like Dr. Rachel Nazarian and Dr. Mona Gohara emphasize that sleep is a "fourth pillar" of skincare alongside cleansing, moisturizing, and sun protection. They recommend:
- Prioritizing 7–9 hours of quality sleep over quantity alone.
- Addressing sleep as a first-line intervention for inflammatory conditions like acne and rosacea.
- Using blackout strategies to protect melatonin, which has direct anti-inflammatory benefits for the skin.
- Integrating sleep hygiene into treatment plans for chronic issues.
Quote from Dr. Gohara: "Sleep isn't optional for skin health—it's foundational. Without it, no topical can fully control inflammation."
How to Reduce Sleep-Driven Skin Inflammation: Evidence-Backed Strategies
-
Achieve Total Darkness to Protect Melatonin
Light exposure at night is a primary inflammation trigger. Use blackout curtains and a reliable mask to ensure zero light leakage.
Why it works: Preserves melatonin's anti-inflammatory role. -
Optimize Sleep Environment for Deep Sleep
Maintain 60–67°F temperature, minimize noise, and avoid screens 1 hour before bed.
Impact: Increases slow-wave sleep, reducing cytokine release. -
Stabilize Circadian Rhythms
Consistent bedtime and morning light exposure align hormonal cycles, lowering baseline inflammation. -
Incorporate Anti-Inflammatory Skincare
Use niacinamide, ceramides, and centella to support barrier repair—especially after poor sleep nights. -
Use a Contoured Blackout Mask for Targeted Protection
Flat masks leak light and press on skin, worsening irritation. A 3D contoured mask like the Nidra Total Blackout Mask provides:- Complete light block without pressure
- Cooler microclimate to reduce swelling
- No fabric contact to prevent microbiome disruption
- Stable fit to minimize arousals
Why Contoured Blackout Masks Are Dermatologist-Recommended for Inflammation Control
Dermatologists prefer contoured masks over silk or flat designs because they eliminate light leaks—the biggest sleep disruptor—while avoiding pressure that exacerbates puffiness and redness. The Nidra Total Blackout Mask is favored for its structured eye cups, which create space for unrestricted REM and prevent heat buildup.
Benefits for inflammation:
- Boosts melatonin by 50%+ compared to partial blackout
- Reduces micro-arousals that spike cortisol
- Supports deeper sleep for cytokine downregulation
- Prevents eye-area irritation from fabric contact
Final Verdict: Prioritize Sleep Quality for Clearer Skin
Sleep deprivation isn't just tiring—it's inflammatory. By focusing on deep, uninterrupted sleep, you can dramatically reduce acne, redness, eczema flares, and sensitivity. Start with total darkness using the Nidra Total Blackout Mask to unlock your skin's natural anti-inflammatory potential.
Dermatologists agree: Better sleep = calmer, healthier skin.
Citations
- Irwin MR. Sleep and inflammation. Biol Psychiatry. 2015.
- Irwin MR. Sleep restriction and inflammation. Sleep Med Rev. 2010.
- Kim H. Sleep and TEWL. Skin Res Technol. 2020.
- Oyetakin-White P. Sleep quality and skin barrier. Clin Exp Dermatol. 2015.
- Van Cauter E. Sleep deprivation and cortisol. J Clin Endocrinol Metab. 2000.
- Fisher G. Cortisol and skin inflammation. Arch Dermatol. 2002.
- Zhang S. Microbiome and sleep. Dermatoendocrinol. 2017.
- Hardeland R. Melatonin anti-inflammatory effects. J Pineal Res. 2009.
- Gooley JJ. Light and melatonin suppression. J Clin Endocrinol Metab. 2011.



Leave a comment
This site is protected by hCaptcha and the hCaptcha Privacy Policy and Terms of Service apply.